Cervical Spine & Motor control : Part 2 DCNF assessment
Here is second part of cervical spine .In case you missed previous blog here is link of part 1
Before we begin I just want to reinforce that motor control is one aspect of cervical spine assessment, which includes:
- Functional assessment
- Observation of posture and active range of movement
- Passive range of movement and palpation
- Neurological assessment
- joint sense error and other tests for sensory motor control
- Motor control.
The author state that “The challenge for clinicians assessing muscular deficits in the cervical region .Additionally, the physical conditioning requirements of patients presenting with mechanical neck pain are not homogenous” (O’Leary, Falla, Elliott & Jull., 2009, p.327).
there is no clear pattern for motor control dysfunctions nor set criteria for normal strength .Therefore, it is important to identify during the subjective examination what patient functional requirements.
It is necessary to observe patient functional task before you begin trying to quantify the motor control strategies. “The observation of dynamic postural control of the cervical spine is not usually directly quantifiable. (O’Leary, Falla 2008)
you should keep in mind while observation at spinal postural.
- How the axio-scapular muscles are functioning.
- what the scapulohumeral position?
- How this changes between weight bearing and not weight bearing positions.
- When observing movement and posture, there is always challenge for the clinicians to link any abnormalities seen to the patient’s neck pain.
ASSESSMENT FOR DEEP NECK FLEXORS:
It is very difficult for deep cervical neck muscles observe and palpate. In 2005, Falla, Jull, O’Leary and Dall’Alba demonstrated that using a nasopharyngeal approach to position EMG electrodes over the posterior oropharyngeal wall was a reliable way to evaluate the function of these muscles without risking injury related to previously used open anterior approach.
ASSESSMENT PROCEDURE……
It is important to screen the craniocervical flexion motion before beginning the test. It’s not strength assessment but the precision and control of muscles.
- The test is performed in crook lying and a towel folded and placed under the patient’s head, so their face is horizontally level.
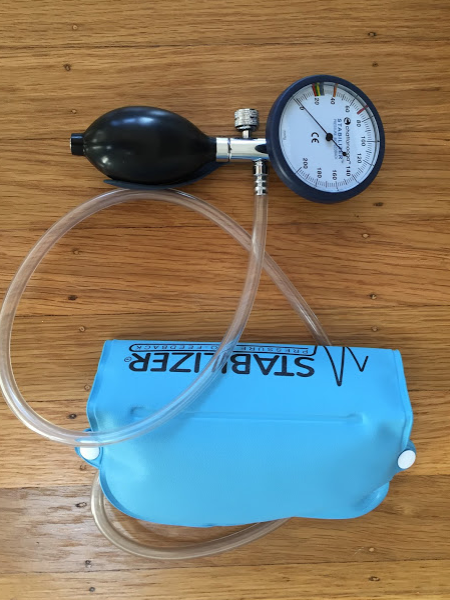
- The towel is placed under the occiput only to allow for the pressure biofeedback unit (PBFU)to be placed under the patient’s neck.
- PFBU is inflated to 20mmHg.
- They should perform a head-nodding movement as if saying ‘yes’ and feel their head slide gently up the towel.
Test 1:
- The first aim is to move the pressure dial from 20-22mmHg. This position is held for 2-3 seconds before relaxing back to 20mmHg.
- The test is then repeated in 2mmHg increments
- The test is stopped when abnormal activity is detected by the clinician which may include:
- Palpable activity of SCM or AS.
- Head retraction or head lifting.
- Increased pressure on the PBFU without increased CCF movement.
- Inability to relax to 20mmHg.
At the end of stage 1 you have gained a ?baseline of the muscle activity. You then move onto stage 2 which is a test of isometric endurance.
Test 2:
- The test is commenced at the lowest level to see if the patient can hold 10 x 10 second isometric contractions at 22mmHg.
- Then they can progress to the next level (24mmHg).
- You should, document the activation score as the level of mmHg by the number of 10 second holds.


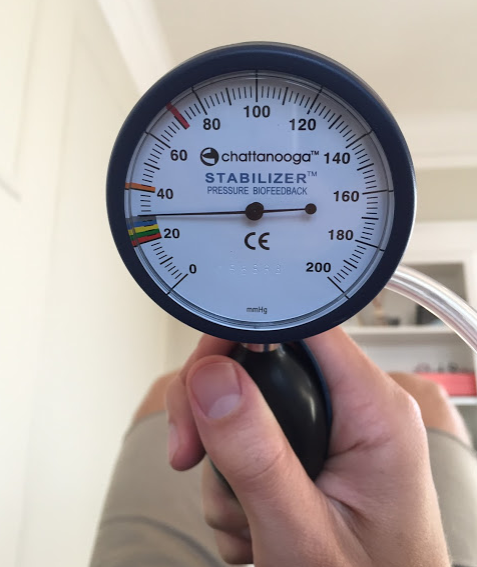
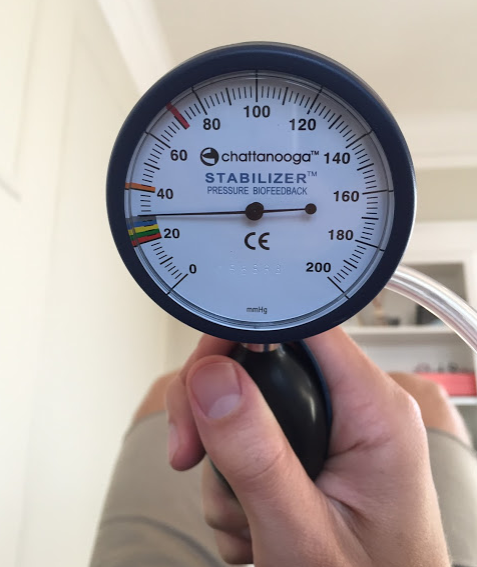
Jull et all(2008) states that It is expected that subjects without neck pain should perform the test to the 3rd or 4th stage i.e. 26-28mmHg.
After completing this assessment, it is advised to reassess sitting cervical extension to evaluate the immediate effect of activation of these muscles on neck pain during active range of movement (Jull, 2008,).
In regards to abnormal test findings One thing that is important to observe the change in neck movement as the test continues. Research shows that the first level 20-22mmHg correlates with 22.9% of available craniocervical flexion. This incrementally increases and in the final stages, 28-30mmHg, 76% of the range should be used” (Jull, O’Leary & Falla, 2008. P. 528). So, if your patient is not able to move further into range of motion then they are not performing the test correctly .The test should be stopped at the previous level they performed well.
we see that patients with chronic mechanical neck pain with higher pain intensity will shower higher levels of superficial muscle activity during the CCFT.
ASSESSMENT FOR DEEP NECK EXTENSORS.
Jull et all (2008),Cervical extensors, both global and local muscles act synergistically to support the weight of the head and produce neck extension.
To assess cranio-cervical extension and finding control of the sub-occipital muscles the patient is position in 4-point kneeling or prone on elbows .
the sub-occipitals, semispinalis cervicis and multifidus are the most changes in their activities. Jull., 2008,and these will be the focus of our ‘deep neck extensor’ muscle assessment.
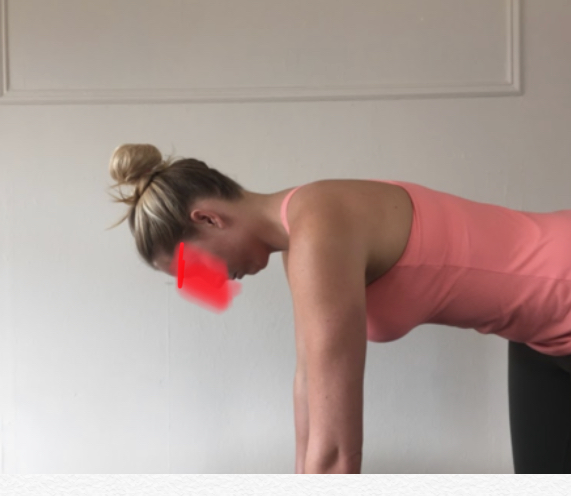

Before the test begins, it is important to ensure that your patient is stabilising correctly otherwise their thoracic and scapulo-humeral positioning can alter the performance of the test. None of the pictures below demonstrate the correct starting position for the test.

Forward head drop

Scapula retraction with forward head drop

Thoracic flexion
As both extensors and suboccipitals are tested in the same position it is important to cue the patient about where the axis of movement is coming from. For the neck extensors (semispinalis cervicis and multifidus) the axis is through the C7 vertebra and the aim is to move their neck while keeping the head-on-neck region neutral.
- The first movement is to curl through flexion and extension using the entire neck.
- If the patient looses control of the cranio-cervical region the clinican will also observe excessive use of the splenius capitus.
- In most cases this test is performed in a pain-free manner (Jull., 2008, p. 176).
- If the patient can’t maintain a neutral cranio-cervical position then the therapist can help to maintain the upper cervical spine in neutral while the patient extends their neck to allow for assessment of the deep extensors (Schomacher & Falla., 2013).
- Documentation of this test is mostly based on observation of quality of movement and length of time/ number of repetitions.

SUMMARY:
You don’t need to get through all the tests day 1, but keep them in your mind and incorporate them into assessments as you progress.
We are still at the stage where strong relationships between posture, altered neuromuscular control, and duration of pain and it’s intensity have not been proven.
“No single test is conclusive or all encompassing in the assessment of cervical muscle function” (O’Leary, Falla, Elliott & Jull., 2009, p.329).
“We have yet to reach consensus about the optimal method of measuring, classifying, and training cervical muscle function” (O’Leary, Falla, Elliot & Jull., 2009., p. 324).
REFERENCES:
- Cleland, J. (2005). Orthopaedic clinical examination: an evidence-based approach for physical therapists. WB Saunders Co.
- ELLIOTT, James M., et al. Differential changes in muscle composition exist in traumatic and nontraumatic neck pain. Spine, 2014, vol. 39, no 1, p. 39-47.
- Falla, D. (2004). Unravelling the complexity of muscle impairment in chronic neck pain. Manual therapy, 9(3), 125-133.
- Falla, D., Bilenkij, G., & Jull, G. (2004). Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine, 29(13), 1436-1440.
- Falla, D., Jull, G., O’leary, S., & Dall’Alba, P. (2006). Further evaluation of an EMG technique for assessment of the deep cervical flexor muscles. Journal of Electromyography and Kinesiology, 16(6), 621-628.
- Jull, G. (2008). Whiplash, headache, and neck pain: research-based directions for physical therapies. Elsevier Health Sciences.
- Jull, G. A., O’Leary, S. P., & Falla, D. L. (2008). Clinical assessment of the deep cervical flexor muscles: the craniocervical flexion test. Journal of manipulative and physiological therapeutics, 31(7), 525-533.
- O’Leary, S., Falla, D., Elliott, J. M., & Jull, G. (2009). Muscle dysfunction in cervical spine pain: implications for assessment and management. journal of orthopaedic & sports physical therapy, 39(5), 324-333.
- O’Leary, S., Falla, D., & Jull, G. (2011). The relationship between superficial muscle activity during the cranio-cervical flexion test and clinical features in patients with chronic neck pain. Manual therapy, 16(5), 452-455.
- Beer, A., Treleaven, J., & Jull, G. (2012). Can a functional postural exercise improve performance in the cranio-cervical flexion test? –A preliminary study. Manual therapy, 17(3), 219-224.
- J. P., O’Sullivan, P., Burnett, A., Barach, A., O’Neil, D., Tveit, O., & Olafsdottir, K. (2010). The influence of different sitting postures on head/neck posture and muscle activity. Manual therapy, 15(1), 54-60.



Leave a Reply
Want to join the discussion?Feel free to contribute!