A Disc Bulge
“Disc bulge” is a term that may have done more harm than the injury itself. How many people hear that word and think, “I’ll never get better” or “my back will never be the same”? As physiotherapists, one of the hardest things we have to do is help people who have hurt their backs get better and convince them that they can and will get better.

Image courtesy of Google Images
“60% to 90% of lumbar disc herniations can be successfully treated with a conservative approach” (Chiu, et al., 2001, p. 185). This is true even though disc herniations are one of the most common causes of back pain. It’s good to hear that!

Image courtesy of Google Images
Medical imaging tests like MRI are used to check out a lot of people at some point. There is always a discussion about whether imaging is clinically necessary to prove a diagnosis and whether it could cause mental harm. We usually send people for an MRI to prove a clinical diagnosis, but it’s interesting that we don’t usually send people for a second MRI after they get better. Still, there are a lot of studies that show people can have disc bulges and not have any pain, other people can have pain without disc disease, and some will get better even if the MRI stays the same. MRI is still a great way to figure out how bad an injury is, but it can also give patients a clear picture of how bad their injury is, which can make them feel bad about their healing and outlook.
In 2014, Chiu and his colleagues did a thorough study to find out how likely it was that a disc would heal on its own. The goal of the systematic review was to find out how likely it is that a disc injury will go away and not come back. In their search, they only looked at research that used mild treatment.
⇒WHAT TO CALL DISC HERNIATIONS
In this study, disc herniations were categorised using words from the “Combined Task Forces,” a body made up of the North American Spine Society, the American Society of Spine Radiology, and the American Society of Neurobiology. In 1995, they came out with a group that had the following:
- bulge
- focal protrusion
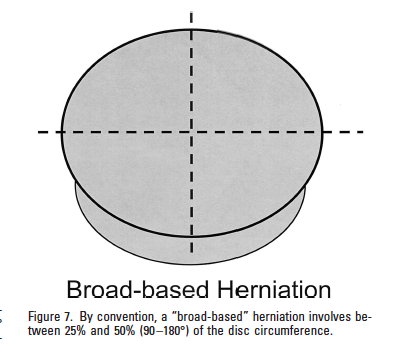
- broad-based protrusion
- extrusion
- sequestration
From this list, it’s clear that the word “bulge” can’t be used to describe all problems. Instead, the word “herniation” is better. “A disc herniation is present if there is localised displacement of disc material and not just outward overlapping, as is the case with some types of bulging” (Fardon & Milette, 2001, p.E100).
“A disc is “protruded” if the largest distance between the edges of the disc material beyond the disc space is less than the distance between the sides of the base when measured in the same plane. Protrusions can be “focal” or “broad-based.” (Fardon and Milette, 2001, p.E100).
“The word “extruded” means to push something from one place to another through an opening in everyday language. Material that was extruded from a disc but has no connection to the disc from which it came can also be called “sequestrated.” (Fardon and Milette, 2001, pp. E100–E101).
According to my internet study and what I know about these scholars, this was the first systematic review on the subject. And that’s what they discovered.


The likelihood of an unplanned regression was
- Disc sequestrations, 96%.
- For disc extrusions, 70%.
- focal protrusions: 41%.
- For disc bulges, 13%.
This indicates that the rate of spontaneous regression is inversely correlated with the degree of disc herniation.
⇒WHY DOES REGRESSION TAKE PLACE?
Three theories are put forward by the writers as to why regression happens:
- When a bulge or localized protrusion forms, the herniation usually retracts to its original place. A technique of dehydration is used to lessen the herniation.
- A disc herniation into the epidural area is more likely to result in an inflammatory reaction.
- Neovascularization and absorption of disc material by phagocytosis and enzyme dehydration are often the results of this.
⇒DISC HERNIATION REGRESSION AND CLINICAL IMPROVEMENT CORRELATION
Because there are so many factors outside the amount of the disc herniation that affect healing, the relationship between disc regression and improvement of clinical outcomes is debatable. Clinical outcomes cannot be predicted by “disc herniation size” or “disc herniation regression” alone. The bigger or more severe herniations frequently have a better likelihood of spontaneous healing, according to the study’s highly optimistic findings.
Summary:
Therefore, you can use the findings of this systematic review the next time a patient has a more severe disc herniation to reassure them (and yourself) that there is a good chance that spontaneous regression will take place and that just because the herniation appears large on the MRI, doesn’t mean they can’t recover.
References
Fardon, D. F., & Milette, P. C. (2001). Nomenclature and classification of lumbar disc pathology: recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine, 26(5), E93-E113.
Chiu, C. C., Chuang, T. Y., Chang, K. H., Wu, C. H., Lin, P. W., & Hsu, W. Y. (2015). The probability of spontaneous regression of lumbar herniated disc: a systematic review. Clinical rehabilitation, 29(2), 184-195.